Deep down in the darkness of calcium and phosphate management and the hormones associated with it requires some information in the field of physiology (the science of the proper functioning of the body), which is below.
How it works
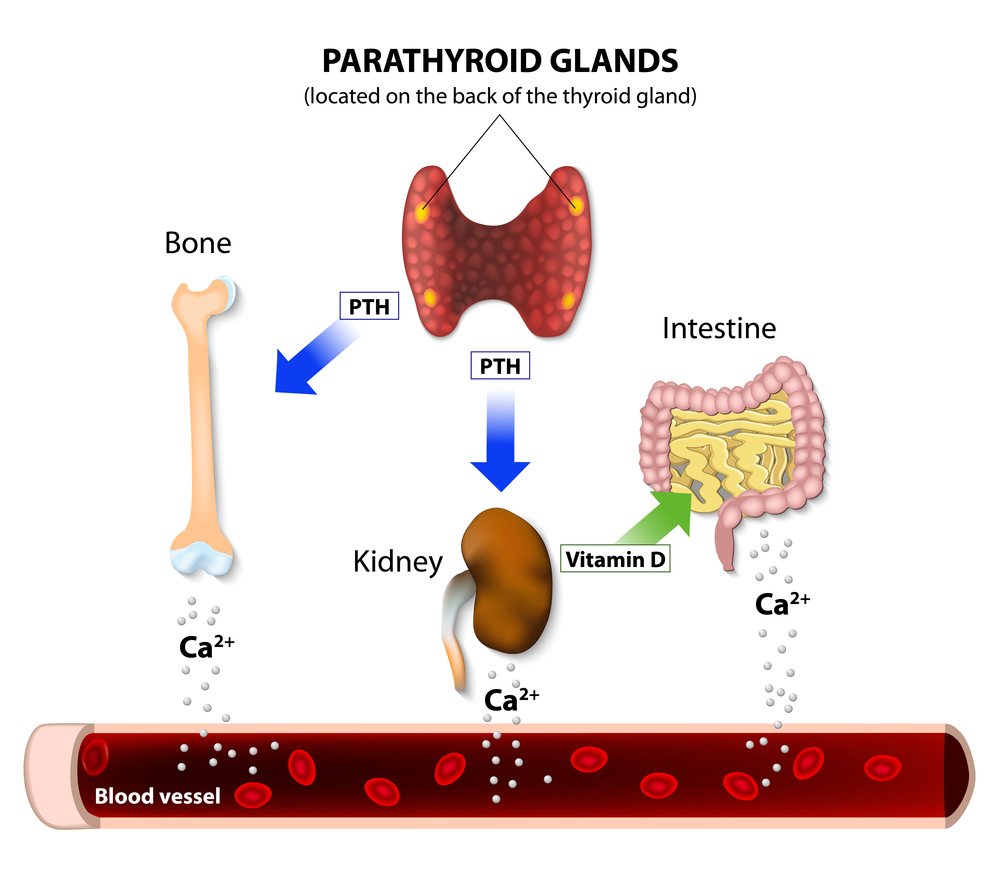
Calcium absorption from the gastrointestinal tract is accomplished with the active form of vitamin D, a hormone called 1,25-hydroxycholecaleferol (it’s also called calcitriol, 1,25-OH-D3).
There is no such problem with phosphates and their absorption, as they can be absorbed without calcitriol; they are also more accessible and common.
The active form of vitamin D is formed from an inactive form mainly in the kidney, under the influence of a hormone called parathyroid hormone (PTH).
Parathyroid hormone is produced by the parathyroid glands - tiny 4-6 glands located, as the name suggests, near the thyroid gland.
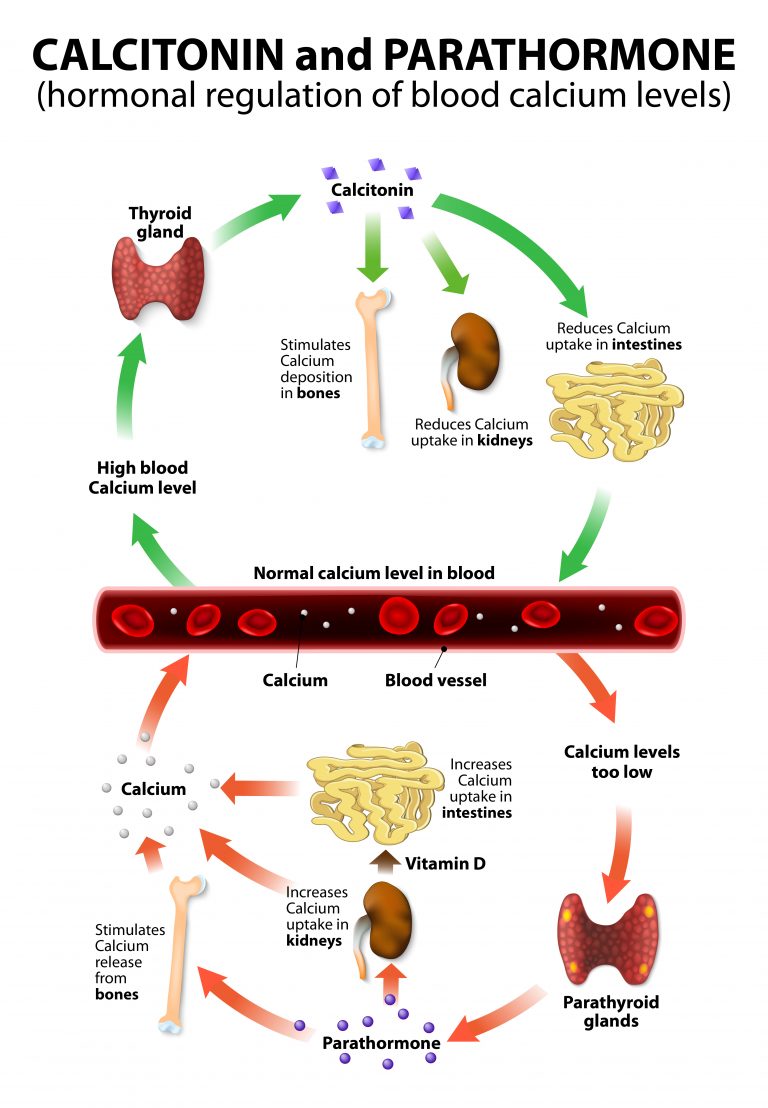
- The production of PTH is primarily influenced by serum calcium level: a decrease in calcium increases the production of the hormone in question, which in turn increases the level of active D3 and calcium absorption. Thus a typical negative feedback loop is created.
- But that's not the end - the increase in PTH levels also causes bone demineralization, calcium release from the bone reservoir
- With phosphate the situation is reversed - the increase in their concentration (indirectly, through a series of multi-step mechanisms, stimulates the secretion of PTH, and this increases the excretion of phosphate through the kidneys.
- The ultimate goal is to standardize calcium and phosphate levels.
It follows that the primary guardian of calcium levels is PTH, which, in pursuit of its behaviour not only (indirectly) increases absorption, but can lead to bone destruction. Why is this happening? Now, calcium is not just bone components, but one of the most important ingredients in many of the compounds necessary for the metabolism of living organisms. Calcium also plays a key signalling role, for example, in a blood coagulation cascade or muscle fibre contraction. Therefore, maintaining the correct level of calcium is a "more important" issue and the body devotes it to the bone.
In the past, the importance of yet another calcitonin-containing calcium-phosphate hormone has been highlighted, but we now know that its role in the calcium and phosphate economy is marginal. This hormone is used, but in the detection of medullary thyroid cancer.
Disorders of calcium and phosphate economy and their symptoms
The above introduction gives you an idea of what the calcium-phosphate disturbance and its hormones may be.
- Calcium and phosphorus deficiency in the diet, although rare, most often show up in people using an amazing slimming diet, will lead to bone demineralization (osteomalacia).
- Vitamin D deficiency or impaired activation, for example due to kidney disease and various medications, also results in the above described complication. This phenomenon is common, especially in old age, when the ability to synthesize vitamin D in the skin under the influence of ultraviolet decreases. Osteomalacia caused by vitamin D deficiency is commonly confused with another bone disease - osteoporosis.
- Excessive activation of vitamin D (sometimes with some cancer and inflammatory diseases) or over-supply (taking it in pharmacological formulations) is a common cause of calcium elevation, which can be manifested by a variety of complaints - from kidney stones to life-threatening dehydration ( Calcium inhibits the ability to thicken urine).
- Parathyroid diseases - hyperparathyroidism (excess of PTH) causes bone decalcification, calcium elevation and many related disorders as described above.
- Parathyroid insufficiency (PTH deficiency) results in decreased calcium and phosphate levels, which is manifested by severe muscle contraction and (paradoxically) the formation of calcium phosphate deposits due to high levels of phosphates.
- Kidney failure is associated with phosphate excretion and vitamin D activation. This in turn increases PTH levels and destroys the bone.
Disclaimer
As we can see, the levels of calcium, phosphate and hormones controlling their economy are influenced by multiple and mutually contradictory factors. Often, hormonal mechanisms are understood to be too simplistic. For example, patients are overconfident about elevated parathyroid hormone levels, interpreted as parathyroid disease. However, an increase in the level of this hormone does not always indicate parathyroid dysfunction, sometimes it is compensatory and is due to other conditions.
Diagnosis of osteoporosis is also abused, which is related to the limitation of inference only to the results of densitometry and other reasons for bone demineralization. The disorders described here therefore require careful examination by the endocrinologist, who should be familiar with the full clinical picture, including the type of diet used by the patient.





2 Comments