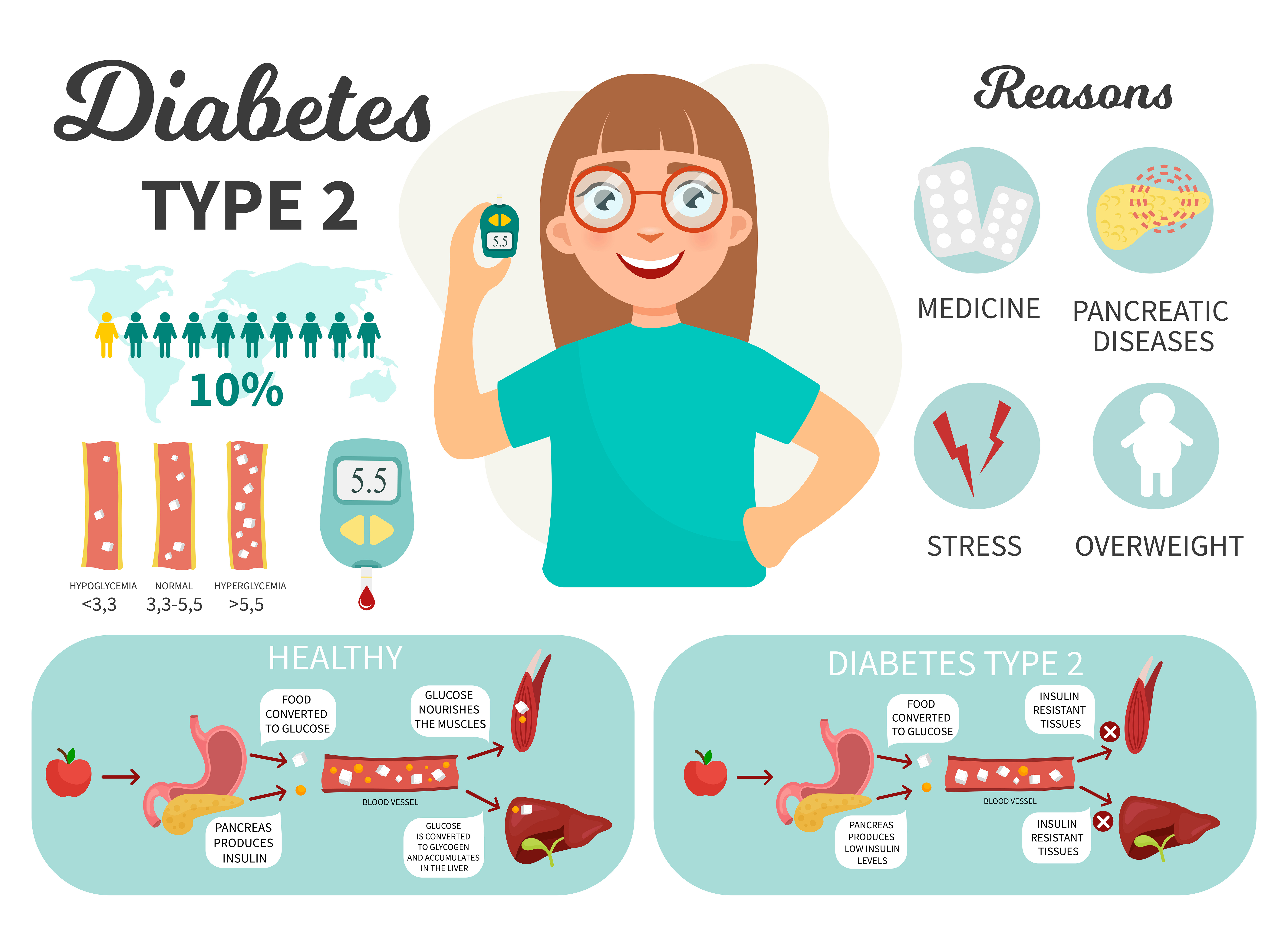
ADA (American Diabetes Association) defines diabetes as a group of metabolic diseases characterized by hyperglycaemia (excess sugar), which is a consequence of disorders of secretion and / or action of insulin. According to GUS data analysed in 2016, the number of ill people in Poland reaches nearly 3 million, with about 90% of cases related to type II diabetes. Type I diabetes was diagnosed in 180,000 people.
Diabetes - new studies
Significant progress made in recent years in the field of prophylaxis and treatment of diabetes caused that despite the disease, diabetics can still enjoy the comfort of everyday life.
Current recommendations increasingly stress the importance of physical activity in the treatment of diabetes, so it’s necessary to thoroughly understand this phenomenon in the context of health safety. For this reason, in this article you will learn, among other things, whether any type of physical activity is indicated in diagnosed diabetes, whether each state of health predisposes to undertake additional physical activity, and whether individually composed perinatal meals can support glycaemic control.
Diabetes and physical exertion
Before an individual physical activity program is established, every patient should undergo a detailed diagnostic assessment. The aim of the study is to determine if there are possible complications from the group of microangiopathies (retinopathy, nephropathy, diabetic neuropathy) and macroangiopathy (ischemic heart disease, stroke, myocardial infarction or atherosclerosis), which may intensify due to extra physical effort . Proper preparation for starting a training plan is therefore crucial to achieve the planned therapeutic effect.
Type 2 diabetes is a special reason why you should take care of your own health. The vast majority of cases of this type of diabetes are diagnosed in people with excessive body mass, leading a sedentary and stressful lifestyle. The disease often develops asymptomatically, slowly damaging the body. That is why it’s so important to introduce additional physical activity, which helps in reducing and maintaining due weight.
According to current medical reports, patients with type 1 diabetes may, just like completely healthy people, do almost any type of sport - unless complications have been diagnosed during the diagnosis. In the event complications, the attending physician will inform you which type of exercise will be inadvisable. It will also be necessary to adjust the doses of insulin analogs and classic human insulins in response to increased glucose consumption during activity. The fact that you have diabetes is not an obstacle to sports.
From a practical point of view, each training should be preceded by a 5-10 minute warm-up including light aerobic exercises (e.g. walking, stationary bikes, trot, etc.) or dynamic stretching (e.g. arm deflections, free foot attacks, dynamic judgments, etc.). It aims to improve circulation and prepare the movement apparatus for the target exercise.
The proper training may include moderate resistance exercises (strength) covering all muscle groups (so-called Full Body Workout), yoga, gymnastics, Pilates or typical aerobic exercises (swimming at swimming pool, running, Nordic walking, brisk walking).
Each training session, just like at the beginning, should end with a 5-10-minute silence session aimed at muscle relaxation and stabilization of the heart rate. Perfect for this purpose is static stretching involving stretching of individual parts of the body or a massage with the help of the popular foam roller.
Diabetes and physical exertion - contraindications
The current state of health is a key aspect in assessing the ability to undertake additional physical activity by the patient. Contraindications that exclude this possibility may turn out to be:
- positive acetone results in the urine, indicating the presence of ketone bodies;
- presence of sugar in the urine exceeding 180 mg%, testifying to glycosuria;
- microangiopathy - retinopathy (damage to the blood vessels of the retina), nephropathy (diabetic kidney disease), neuropathy (damage to the nervous system). Contraindications concern specific sports disciplines, which are decided by the attending physician;
- blood sugar below 100 mg%, which, combined with additional effort, can lead to hypoglycaemic coma;
- blood sugar levels exceeding fasting 250 mg% in combination with the occurring ketosis;
- lack of balanced diabetes, which is manifested by significant variations in sugar during the day;
- ischemic heart disease with coronary pain at the minimum of even physical exertion, often coexisting with diabetes in the form of metabolic syndrome.
Post workout meal in diabetes - examples
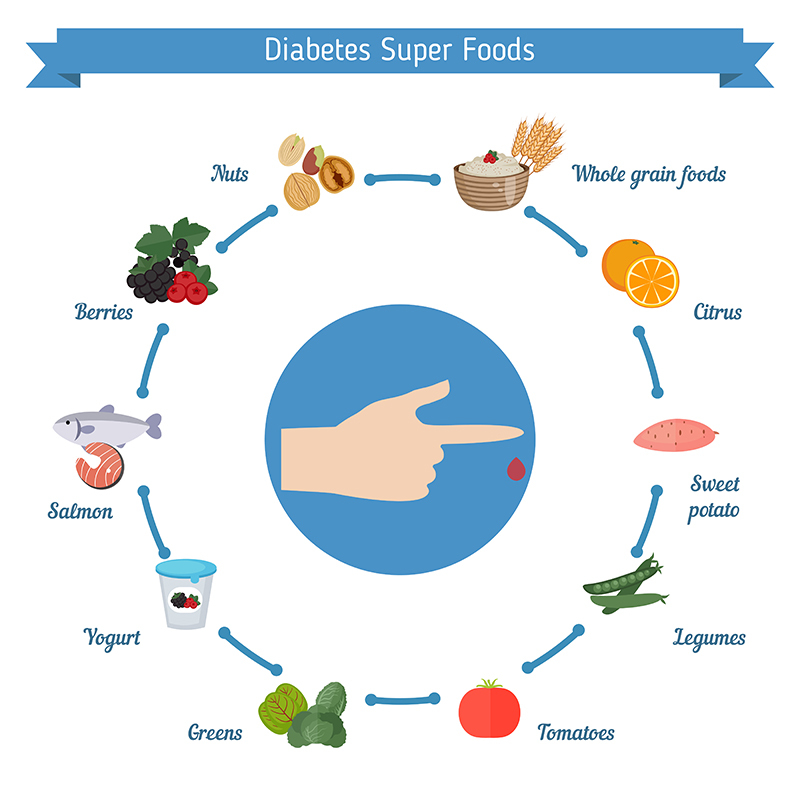
An extremely useful "tool" in regulating the glycemic response to exercise is a properly composed daily diet, especially taking into account the post-workout meal. Depending on the blood glucose level, patients should learn with their doctor or dietitian how to use insulin doses and how to plan carbohydrate meals. To avoid hypoglycaemia, a carbohydrate-containing meal should be delivered immediately after the training unit has finished. Ideal in this case will be a composition of easily and slowly assimilable forms of carbohydrates with an additional portion of protein and less fat.
Example of meal:
- natural yoghurt (source of animal protein and fat)
- chia seeds (source of fibre, vegetable protein, pro-health omega-3 fatty acids)
- oatmeal (a slowly absorbable form of carbohydrates with a low glycaemic index)
- two slices mango (easily digestible form of carbohydrates with an average glycaemic index, source of vitamins and minerals).